Home / Useful Resources / Finding the Right Surgeon
Finding the right surgeon
Before you schedule surgery or any treatment, you need to feel confident that your specialist or surgeon is right for you. It is important that your surgeon listens to and fully answers your questions, so that you can understand why surgery has been recommended and what will be involved in each step of preparation and recovery. To know more about potential questions that you may ask your surgeon during your first visit, look here.
Additionally, a successful procedure relies on good communication that builds trust and leads to better results and overall satisfaction. It also helps your doctor and health care team to get to know you better and vice versa. The right surgeon will be committed to this two-way relationship.
You may also consider speaking to other patients or medical professionals about the surgeon or specialist with whom you are considering treatment.
To read more on patient experience stories, you may look here.
Roles of the Care Team
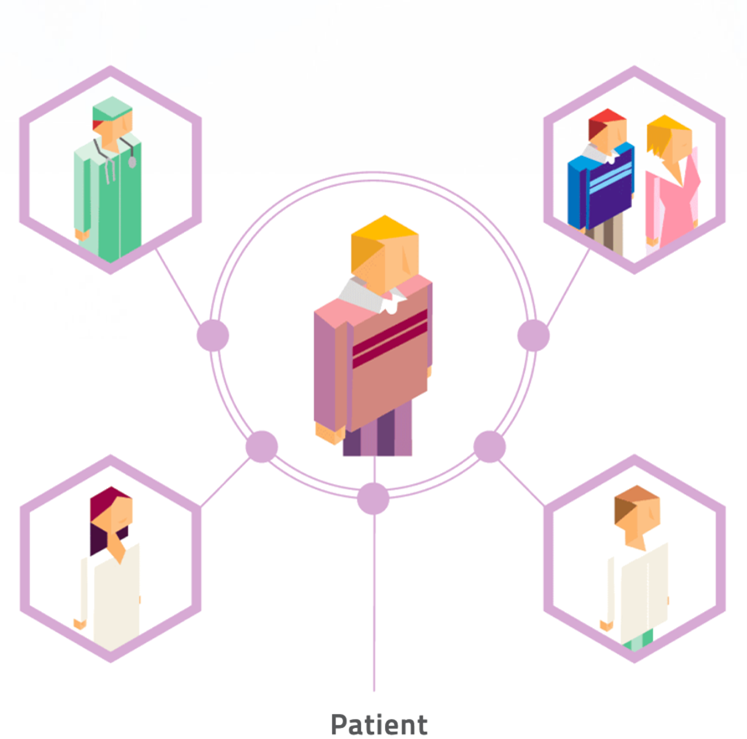
Patient
You are the most important member of the care team and will need to be active in the process, both before and after surgery, to help your limb heal. Tasks will include preparing for the surgery and taking care of your limb after surgery by performing physical therapy exercises, tending to the surgical site wound and other important steps as instructed by your surgeon and members of your care team. You should also ask questions to ensure that you fully understand each step of the way and to help your care team meet your needs. Share your concerns so that your surgeon, nurses and physical therapist can make your recovery as smooth as possible.
Surgeon
Your surgeon will be with you beyond the initial evaluation and surgery and will help you create a recovery plan. The surgeon and their team will follow up with you at certain times to ensure that your treatment is progressing as intended.
Family and Friends
You will need help at home along the way. Involve your family or close friends from the start so that they can understand the procedure as well as you do. Your family and close friends may be able to help you plan for the surgery and recover from it; for example, they may help you with physical therapy exercises.
Hospital Team
Nurses and other medical professionals in the hospital will assess your health status before surgery. They will coordinate your hospital stay on the day of surgery and after surgery. Their role is to guide you through each phase of your treatment until you are able to go home. The nursing staff will help control your pain and teach you about caring for yourself after surgery. Don’t be afraid to ask your nurses questions about the surgery process or to express your concerns before or after surgery; nurses can help you with and advise you on a range of issues.
Physical Therapist
Your physical therapist will assess your movement ability before surgery and work with you throughout the process to help you stay as active and independent as possible. After surgery, the physical therapist will teach you exercises to do both in the hospital and at home, and give you a plan for getting you back on your feet. You may see the physical therapist on a regular basis to assess how you are progressing and to make any changes to the plan.
Pre-operative consulation
Here are some considerations to work through with your surgeon as part of planning for your surgery. Questions to ask your surgeon during your first pre-operative visit may be found here.
Checklist of Information Your Surgeon May Ask You to Provide
During your first visit with your surgeon and their team, you may be asked to provide some information regarding your condition and health status. The following is a checklist to help give an idea of what may be expected:
Treatment Options
Before deciding on surgery, your surgeon will explain your treatment options. There are a variety of non-surgical and surgical treatment options that may be appropriate, depending on the type and extent of your limb deformity. For more info look here.
What type of orthopedic device have you been prescribed?
If your physician or orthopedic surgeon has assessed your treatment needs and has decided that surgery for the application of an orthopedic device is the best treatment for you, you can find some more information here about the various types of devices currently available for limb deformity correction. Feel free to discuss your surgery with your doctor and the advantages/disadvantages of the orthopedic device they have recommended for you.
External Fixators
External fixators are devices that are attached to the bones of the limb that is being corrected. A major portion of these devices are outside of the body with a small portion on the inside of the body attached to the bone.
The number of external fixator devices that a single patient receives depends on the surgical case; this will be conveyed to the patient by the doctor.
While the deformity is being corrected, the external fixator will need gradual adjustments to help new bone tissue grow into place over time. When your surgeon is happy with the length, shape and alignment of the bones, adjustments will no longer be needed.
You will still wear the external fixator after adjustments are complete to support your limb while the new bone hardens and the limb becomes stronger. A good rule of thumb to remember is that consolidation takes twice as long as lengthening/reshaping. Look here for understanding how limb correction works.
The amount of time the external fixator will be in place depends on the severity of the deformity, and how much correction is needed, as well as your general health and medical history. An external fixator is usually in place for 4 to 12 months.
After the new bone has fully solidified, the external fixator is typically removed during an outpatient surgical procedure (the patient does not have to stay in the hospital overnight for this).
For some experts, external fixation is based on a minimally invasive concept as it requires minimal excision and all the metal of the frame is removed at the treatment’s end.
The two main types of external fixators used for limb deformity correction are:
Circular external fixators can completely or partially encircle the arm, leg or foot that is being corrected. These fixators are made up of two or more circular rings that are connected by wires or pins. The patient (or family member) may need to adjust the device several times a day by turning knobs (for more specific info on the post-surgery care, look here).

Monolateral external fixators have a straight bar that is placed on one side of the arm, leg or foot. It is connected to the bone by screws that hold the bone and prevent loosening.

Internal Fixators
Internal fixation is when the device corrects the bone by being completely inserted inside the bone.
The advantages of internal fixation include shorter hospital stays and enabling you to return to normalcy sooner as compared to other methods. During the surgery, the doctor implants the internal fixator device to keep the bone in the corrected position as it heals.
The main types of internal fixator devices used for surgical limb correction treatment are:
Plates are splint-like devices that hold the separated segments of bone together. They are fixed to the bone using screws. Plates may either be left in place after healing is complete, or in some cases, they may be removed.
Guided growth plate is an eight-shaped device that allows gradual correction of the deformity in children, provided that the physis (growth plates) are not fused. This type of surgery is called hemi-ephiphysiodesis. Epiphysiodesis is a Greek term in which “physis” means growth plate and “desis” means tether.
The plates are attached to the external surface of the bone over the growth plate by screws. These screws are not locked to the plate, but rather are allowed to swivel and diverge in their position as bone growth occurs. The implant acts like a flexible hinge, permitting growth at the growth plate to gradually straighten the limb. The goal is to permit realignment through growth. More simply put, bone growth is restricted on one side of the deformity while bone growth continues on the other side. Gradually, the bone realigns and the deformity is corrected.

Nails and rods are both inserted into the center of the bone. The difference between the two is that only nails are attached to the bone with cross bolts or locking screws. A nail has small holes drilled at both ends through which screws or pins are inserted that help stabilize it to the bone. Rods are inserted inside the bone, but are not attached to the bone with bone screws or pins. Rods tend to be more flexible and thinner than nails.
For the correction of long bones (such as the femur or tibia), one of the most efficient ways to hold separate segments of bone together is by inserting a rod or nail within the affected bone. The doctor uses an orthopedic drill to create a canal in the hollow center of the bone known as the intramedullary canal (that contains bone marrow). This canal will be large enough for the nail or rod device to be inserted. Screws present at both ends of the nail help to keep the bones stable until complete healing occurs.
Recent advances with minimally invasive surgical techniques have allowed patients to regain independence much faster than before. Here, the intra-medullary lengthening nail is completely implanted in the bone as a keyhole operation; in other words, as a minimally invasive procedure with only tiny cuts. This has several advantages for the patient: small-to-very small scars, no external fixators and no risk of infection at the body exit points.

A lengthening nail differs from a standard intramedullary nail. It consists of a telescopic metal body with a motor inside of it. The bone is cut in the middle prior to the insertion of the lengthener. Since the nail is inserted into the hollow canal of your bone, called the intramedullary canal, the orthopedic surgeon will use an orthopedic drill to create the space in the bone for the device to fit inside it.
The surgeon operates through a very small incision and the hospitalization is generally very short, from one to three days maximum. The intramedullary nail is fully implantable, which means that, in comparison to the external fixators, nothing sticks out of the patient. It is connected to a receptor positioned just under the skin and this receptor will receive a signal from an external source, which will then be transformed through a transductor to electrical energy within the device. This will allow the lengthening of the nail and of the patient’s bone. The patient (or family member) may need to repeat this action several times a day (for more specific info on the post-surgery care, look here).
Look here for understanding how limb correction works.

Screws are the most common internal fixators used for orthopedic surgical procedures. They may either be used alone to hold together two segments of a bone, or can be combined with plates, rods, or nails. After healing is complete, screws may be left in place or removed.

Wires and pins are used to hold together segments of bone that may be too small to adjust with screws. They may either be used in combination with other internal fixation devices or can be used alone to treat fractures of small bones, such as those found in the hand or foot.
Being aware of possible complications
If surgery is the best option for the correction of your limb deformity, your surgeon will explain the reasons it has been recommended. In addition, the surgeon will provide complete details of the surgery, including its benefits and risks. It is important to remember that all surgeries come with certain risks.
Following are some risks to be aware of and ask questions about, if you have any concerns.
General Complications That May Occur with Limb Deformity Correction Surgeries
Depending on whether you will receive an external or internal fixator device, the following is a list of additional, procedure specific, adverse effects that exist for these kinds of surgeries.
Complications That May Occur with External Fixation
Complications That May Occur with Internal Fixation
At the end of treatment, the deformity or the original problem may not be completely cured and you may still have some symptoms. It is best to discuss this with your surgeon who can provide you the best information and guidance on the expected success rate for your procedure.