Home / Useful Resources / Early Detection
The early signs of an orthopedic condition may be detected in children at birth or over the course of their early years up until their teenage years. Other than the child’s pediatrician, you – the parent – also play a significant role in detecting the condition early on.
The best time to consult your doctor is whenever you, as the parent, feel that something is not right with your baby or child in terms of posture, movement or any other signs. The earlier a bone deformity is diagnosed, the more successful the treatment will be.
The age at which symptoms present themselves varies from child to child. Some bone deformities are evident at birth, such as clubfoot, while others may present themselves between 10 and 18 years of age, such as scoliosis. To learn more about various orthopedic conditions that may affect children, you may look here.
During your doctor’s visit, the doctor will carefully examine your child and explain to you in detail the child’s diagnosis (if any). Additionally, they will explain the best treatment option that is appropriate for the child. For more information on surgical and non-surgical treatment options, you may look here.
The doctor may also request for additional X-rays, blood and/or nerve tests to assist with their diagnosis. It is important that you feel comfortable asking your doctor any questions about your child’s diagnosis and treatment. The better informed you are, the more comfortable you and your child will be during the course of treatment. You may look here for more guidance on finding the right surgeon.
The younger a child is, the more flexible their bodies are, making early detection a challenge sometimes. However, a parent’s intuition is a great indicator and if you feel something is “just not right,“ then you should book an appointment with your pediatrician and get your child examined. During your child’s routine checkups, the pediatrician does a series of tests by moving the child’s limbs in a certain manner to look for characteristic signs of some orthopedic conditions. However, as a parent, you may also want to look out for certain indicators as well.
Signs to look out for include (but are not limited to):

With the increasing prevalence of diabetes in the world, patients need to be aware of early detection signs in the feet for diabetes related orthopedic complications.
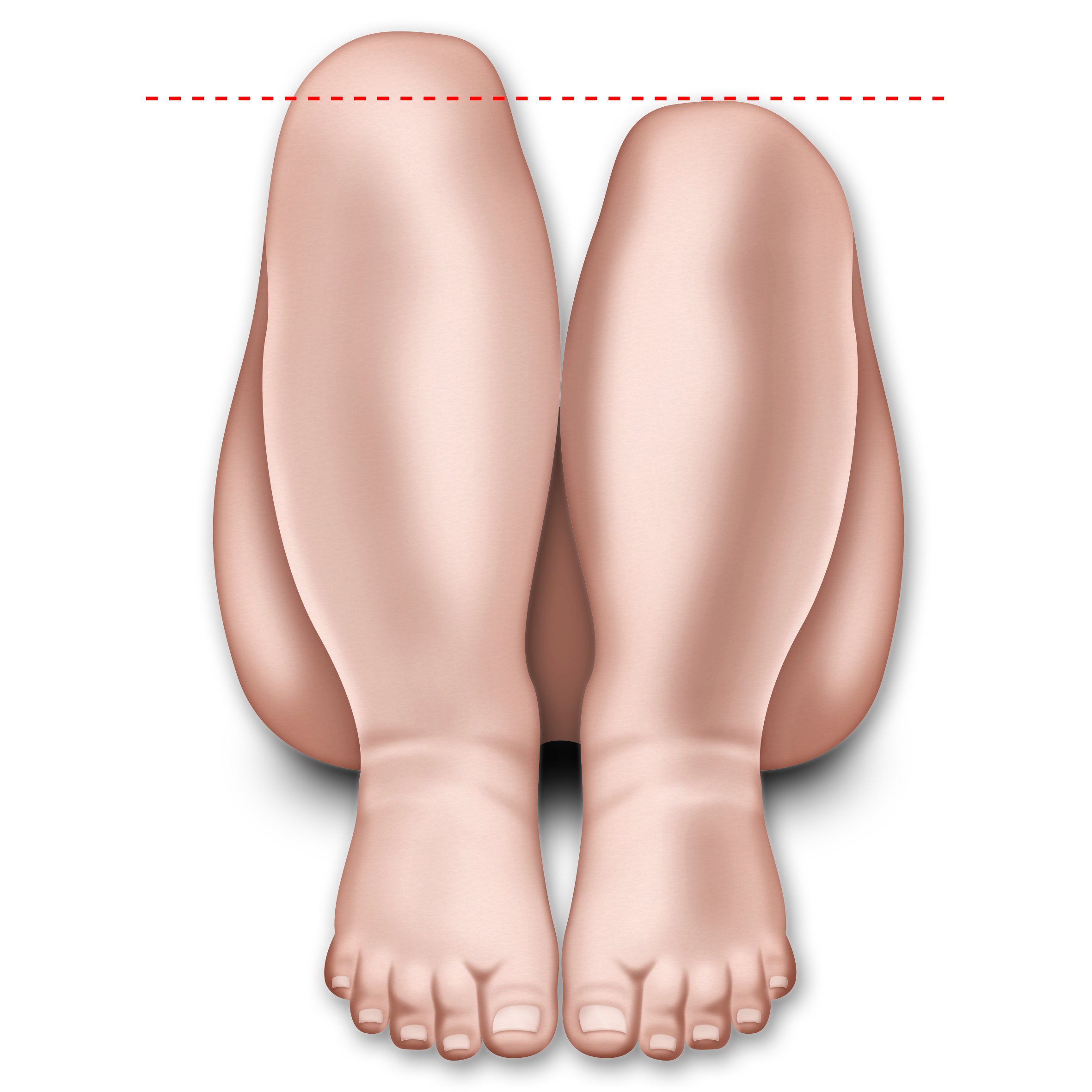
0.3% to 7.5% of diabetic patients may develop a Charcot neuroarthropathy. Diabetic neuropathy (i.e. nerve damage) and peripheral vascular disease (i.e. poor circulation) are two of the main foot problems that occur, and both can have serious complications. If left untreated, this condition leads to deformity, ulcers and infection and – in the worst case – to amputation. Worldwide, 85 percent of leg amputations are a result of a diabetic foot ulcer. Up to 80% of diabetic patients are more likely to die within 5 years of having a limb amputation. However, 4 out of 5 amputations can be prevented. Timely diagnosis facilitates treatment and decreases long-term disability. Therefore, it is essential for diabetic patients to be aware of the early detection signs for diabetes related foot problems.
Nerve damage and poor circulation in the feet may lead to numbness or lack of sensation. This means that if a patient with diabetic foot develops an ulcer or infection in their foot, they would not be able to recognize it as the sensation of pain or irritation is largely reduced or completely absent. They would not realize that their feet require medical attention. This unintentional ignorance may lead to a buildup of gangrene, which, if left untreated, leads to a possibility of foot amputation as a worst case scenario.
Complications of diabetic foot problems include:
Your role is key in preventing and reducing complications by:
If you notice any of the following changes, you should seek immediate medical attention:
Non-surgical: the first attempt would be to treat a diabetic foot without using surgery. This is possible if the condition is caught early on. Some methods include:
Surgical: when non-surgical treatment does not successfully heal diabetic foot problems, the doctor might consider surgery. Many new surgical techniques are available to avoid amputation, such as joint reconstruction and wound healing technologies. Regular checkups with your doctor may help catch problems at an early stage, which is crucial to get effective treatment. A proactive approach by the patient is crucial; visit your doctor as soon as a symptom is observed. Surgical treatment options include:
Even with preventive care and prompt treatment of infection and complications, there are instances when amputation is necessary to remove infected tissue, save a limb or even save a life. Amputation, ranging from single toes or sections of foot to amputation of the leg below or even above the knee, is the worst case scenario and requires the surgeon to remove the infected portion of the leg to avoid further spread of infection.