Internal fixation is when the device is used to lengthen the bone from inside the bone. After insertion, the patient will stay in the hospital for about 2 to 3 days.
Physical therapy is crucial as it allows for the muscles, tendons and ligaments to be stretched in order to ensure that the arm or leg will have full movement after treatment. Patients will need physical therapy if they are lengthening the bones in the legs or occupational therapy if they are lengthening the humerus (upper arm bone).
The patient will be allowed only limited weight bearing on the affected limb. The doctor will determine how much weight bearing is allowed and the size and type of the nail that is implanted. If both legs are to be lengthened, a wheelchair would be required for the post-surgery healing phase.
Some pain and swelling are expected post-surgery. Your doctor will prescribe pain killers and other medication to help make the post-operative phase as comfortable as possible.
The following are some guidelines to keep in mind post internal fixation surgery.
Activity
- Good quality sleep is a great recovery tool. Try and rest whenever you feel tired.
- Increase your activity only as recommended by your doctor.
- Avoid putting weight on your repaired bone until your doctor says it is okay.
- You may need to take 1 to 2 weeks off from work. It depends on the type of work you do and how you feel.
- Do not shower for 1 or 2 days after surgery. When you shower, keep your dressing and incisions dry. If you have a cast, tape a sheet of plastic to cover it so that it does not get wet. It may help to sit on a shower stool.
- Do not take a bath, swim, use a hot tub, or soak your affected limb until your incision is healed. This usually takes 1 to 2 weeks, but will be specified more clearly by your doctor.
Incision Care
You may have a tape placed on the site of incision. This is to be kept in place until the doctor allows you to remove it or until it naturally falls off. When your doctor allows you to remove the bandage, you may clean the incision site per your doctor’s instructions.
Ice and Elevation
You might be asked to prop up the injured arm or leg on a pillow as you ice it or anytime you sit or lie down during the first 1 to 2 weeks after your surgery.
Other Instructions
If you have a cast or splint, it is advisable to:
- Keep it dry.
- If you have a removable splint, ask your doctor if it is okay to take it off to bathe. Your doctor may want you to keep it on as much as possible. Be careful not to put the splint back on too tightly.
- Do not stick objects such as pencils or coat hangers in your cast or splint to scratch your skin.
- Do not put powder into your cast or splint to relieve itchy skin.
- Never cut or alter your cast or splint.
Follow-Up Care is a Key Part of Your Treatment and Safety
Be sure to make and go to all appointments and call your doctor or nurse call line if you are having problems.
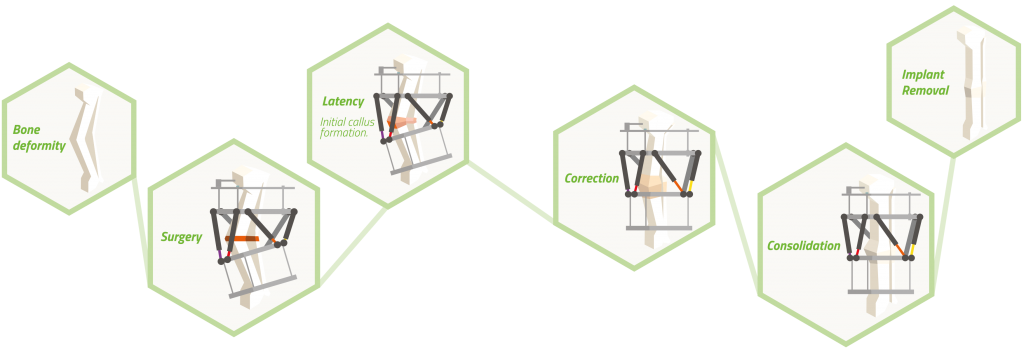
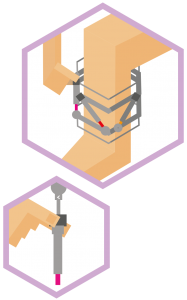
Deformity Correction with a Guided Growth Plate
Implantation of a guided growth plate is performed under anesthesia and takes about an hour. During the procedure, the surgeon will make a 2-3cm (approximately 1”) incision at the physis of the bone to correct. The plate is secured to the bone with two small screws. The incision is closed, generally with resorbable sutures. After recovery from anesthesia, your child may be taken home. This technique involves minimal surgical trauma and pain when compared to an osteotomy. Although your surgeon will provide details on your child’s specific case, a cast is generally not required and crutches are usually optional (for comfort). Subject to your surgeon’s medical judgment, typically children are encouraged within three weeks from the surgery date to walk and resume activities as tolerated.
The guided growth plate temporarily restrains growth on one side of the bone plate while natural growth is allowed to continue on the opposite side. Gradually over time, (typically from several months up to one year) the deformity is corrected. To ensure timely and adequate correction, your child needs to be seen by the surgeon every three months for a check-up or as recommended by your surgeon. When the deformity is corrected, the surgeon will remove the guided growth plate under anesthesia in an outpatient surgery.
Limb Lengthening with a Nail
If you have been treated with a lengthening nail, your surgeon will explain the schedule and how many visits will be needed.
A load of up to 20 kg on the affected leg is typically permitted. Stacked shoes are used to compensate for differences in leg length. Physical therapy is initially limited to the prevention of pulmonary and thromboembolic complications. Exercising of the knee joint typically starts from the fourth post-operative day. Always follow the physical therapist’s instructions.
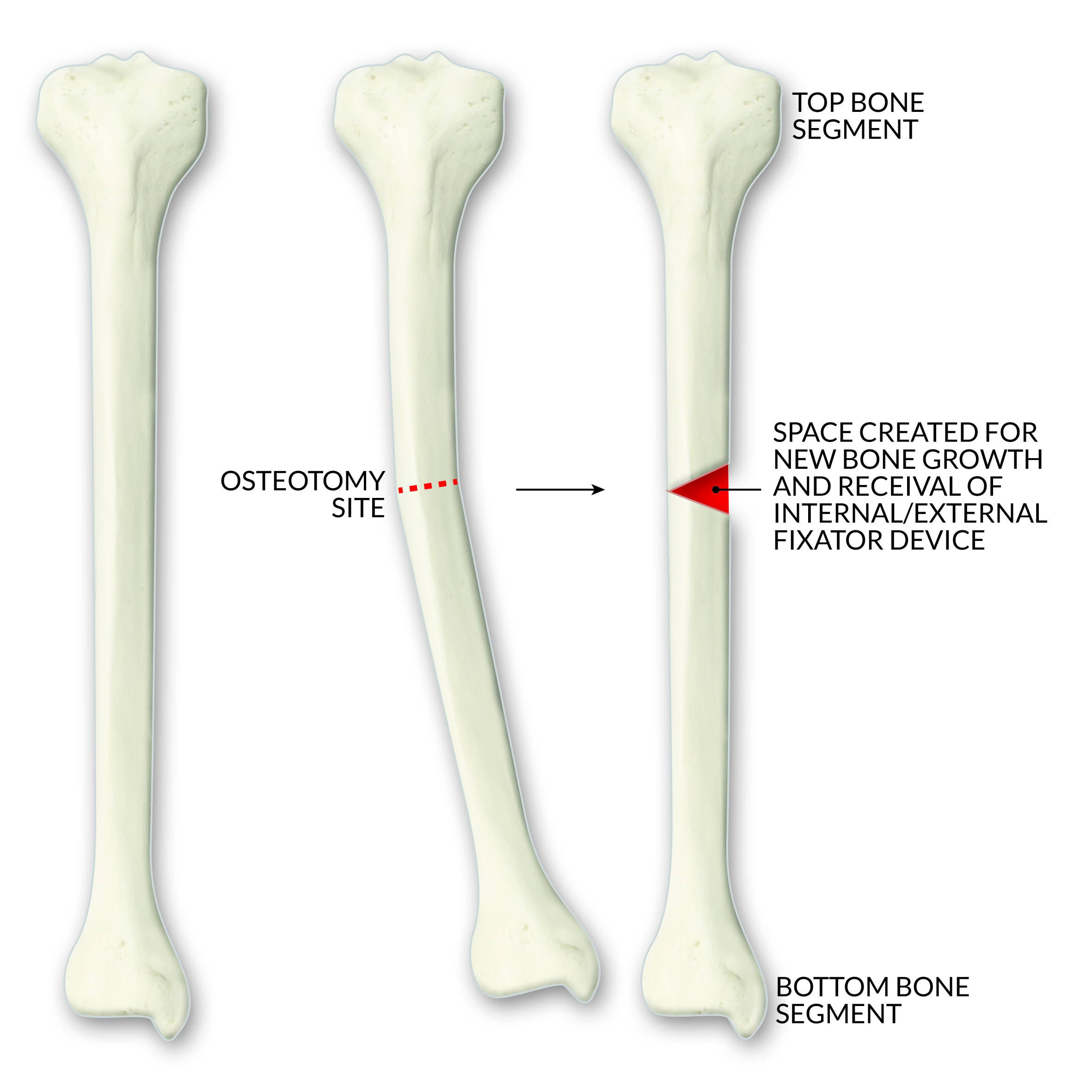
The distraction phase will typically start 5 days after your/your loved one’s surgery. Your surgeon will give you a special device and you will be shown how to use it to activate the motor inside the nail. This will allow the lengthening of the nail and of your bone.
You may need to repeat this action several times a day to reach the planned bone lengthening as prescribed by your surgeon. This allows lengthening of your bone at a comfortable rate, letting your new bone grow in the surgically created space. Lengthening too fast may mean that new bone cannot grow fast enough and this will cause problems with bone healing. Lengthening too slowly may result in the bone growing together before lengthening is done.
By taking regular X-rays of your bones, your doctor will ensure that the lengthening isn’t happening either too fast or too slowly. Your doctor may ask you to change the rate of corrections as a result.
When the distraction is complete and the correct leg length is attained, the soft regenerate begins to calcify into hard bone. Your surgeon will use X-ray pictures of your limb to determine when your bone has hardened enough to allow you to place all your weight on your leg again. After that time, you may choose to have the device removed from your leg with another surgical procedure.