Home / Limb Deformities / Perthes Disease
Perthes disease is a rare childhood condition that affects the hip joint. The full name for the condition is Legg-Calve-Perthes disease (LCPD), and it is also known as coxa plana. It affects boys more frequently than girls, and can be diagnosed between the ages 3 and 12. 1
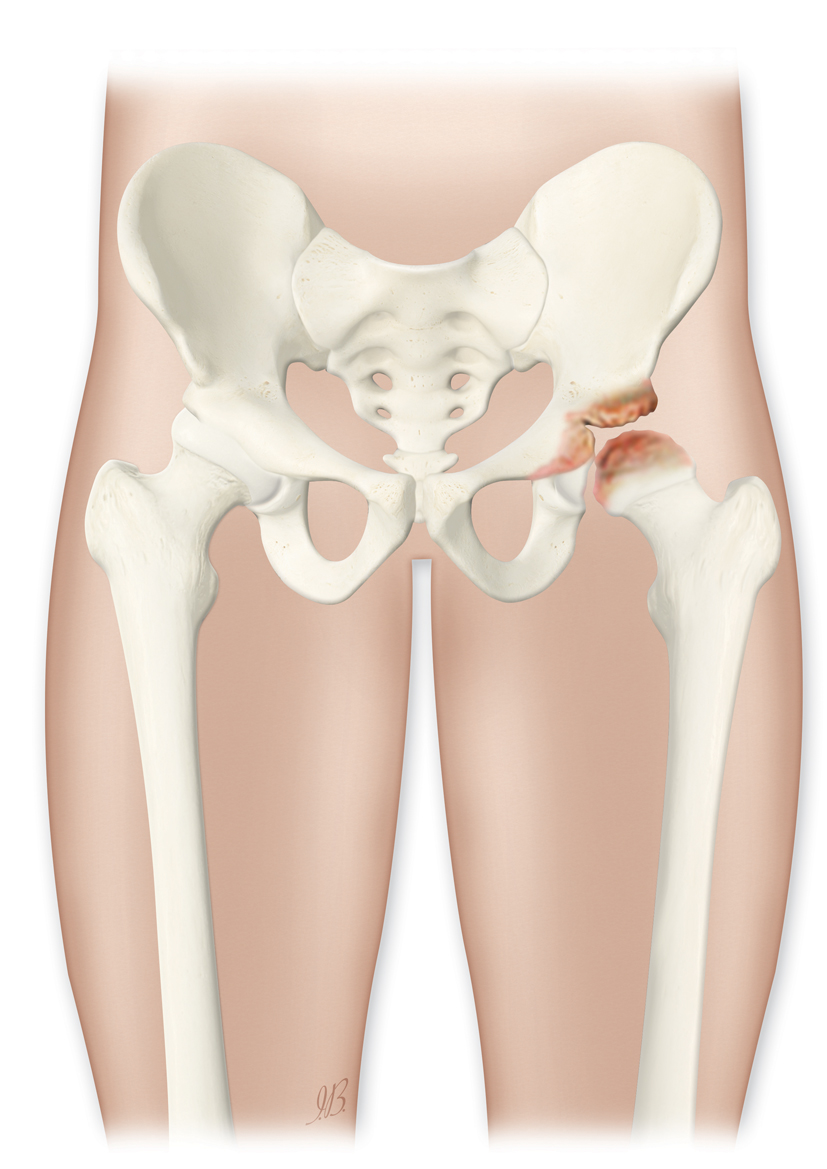
Perthes is a complex process of four stages that can last from 2 to 5 years. As the condition progresses, the weakened bone of the ball of the hip joint, the femoral head, gradually begins to break apart. Over time, the blood supply of the femur returns, and the bone starts to remodel and recover.
The outlook is favorable for children who develop Perthes disease at a younger age because the hip joint has more growing time to remodel into the normal round shape. Children who develop the condition later (after 6 years of age) are more likely to have hip problems in adulthood.
Important safety information: Download the Product Instructions For Use.
The Guided Growth System eight-Plate and quad-Plate is an implant system designed to correct pediatric deformities (congenital or acquired) in lower limb, like genu valgum and varum, and limb length discrepancies. The plates are attached to the external surface of the bone over the growth plate by two or four screws depending on the plate selected by the surgeon. The implant acts like a flexible hinge, permitting growth at the growth plate to gradually straighten the limb when the physis (growth plates) are not fused. The screws are not locked to the plate but rather are allowed to swivel and diverge in their positions as the bone grows. Immediately after implantation, the patient is allowed mobility and weight bearing.
Important safety information: Download the Product Instructions For Use.
The eight-Plate Guided Growth System+™ is an implant system designed to correct pediatric deformities (congenital or acquired) in lower limb, like genu valgum and varum, and limb length discrepancies. The plates are attached to the external surface of the bone over the growth plate by two or four screws depending on the plate selected by the surgeon. The implant acts like a flexible hinge, permitting growth at the growth plate to gradually straighten the limb when the physis (growth plates) are not fused. The screws are not locked to the plate but rather are allowed to swivel and diverge in their positions as the bone grows. Immediately after implantation, the patient is allowed mobility and weight bearing. The eight-Plate Guided Growth System+ offers more sizes and different screw types compared to the standard eight-Plate Guided Growth System, as well as an increased screw angle to treat very difficult cases.
Important safety information: Download the Product Instructions For Use.
The FitboneTM Intramedullary Limb-Lengthening System was developed in partnership with Professor Baumgart. The product was launched in 1997. Since then, this innovative treatment concept has grown into a global success story. The Fitbone TAA Intramedullary Lengthening system is intended for limb lengthening of the femur and tibia. With appropriate pre-operative planning, it is possible to ensure good limb alignment so that the limb is correct at the end of lengthening.

The cause is unknown, but it may be related to a disruption in the blood supply to the ball of the hip joint, the femoral head. Research is continuing to understand why some children are affected but not others. Theories include a genetic predisposition, and there may be an association with secondhand smoke.
One of the earliest signs is a change in how the child walks and runs. Typical symptoms are pain, limping, or stiffness in the hip, groin, femur or knee, which is exacerbated by activity. The child may become unable to bear any weight on the leg.
A limited range of movement in the hip joint is common, as well as painful muscle spasms. The condition generally involves just one hip, but in some children, both the hips are affected, usually at different stages. 2

Perthes disease should be considered in all children who present with a limp or pain on activity.
After examination of the hip for range of movement and pain, hip X-rays may be performed as these can show changes of the disease at an early stage. In some cases, MRI scans may be used to show bone marrow changes.
The doctor’s treatment plan depends on the child’s age, the condition of the femoral head and the stage of the condition when the child is diagnosed. Treatment may last from 18 months to 2 years, and its goal is to obtain a spherical and congruent hip at skeletal maturity.
For very young children (2-6 years old) therapy may include simple observation (“watch and wait”), rest, with regular monitoring through X-rays, and physiotherapy advice to maintain hip movement and functional improvement. 3,4
A minor operation to release the tendon on the inside of the thigh, the adductor tendon, may be required. Some centers also then use a cast or brace to spread the hips apart in the optimum position. 5
For some, especially older children, surgery may be needed to alter the shape of the hip socket or modify the position of the femoral head within the socket. The affected bone will be re-oriented through a controlled fracture, or osteotomy, and then held in the new position with screws and plates. 6 ,7,8

In most cases, the long-term prognosis is good. There may be a small leg length difference that requires surgical treatment or a shoe modification to prevent future problems.
Children affected by Perthes disease are at a higher risk of hip arthritis in adulthood, especially if the healed hip bones do not fit well together. This is more likely in older children, and in those who had a greater deformity and collapse of the femoral head.
Any surgical treatments have their own risks including infection and metalwork problems.