Home / Limb Deformities / Leg Length Discrepancy (LLD)
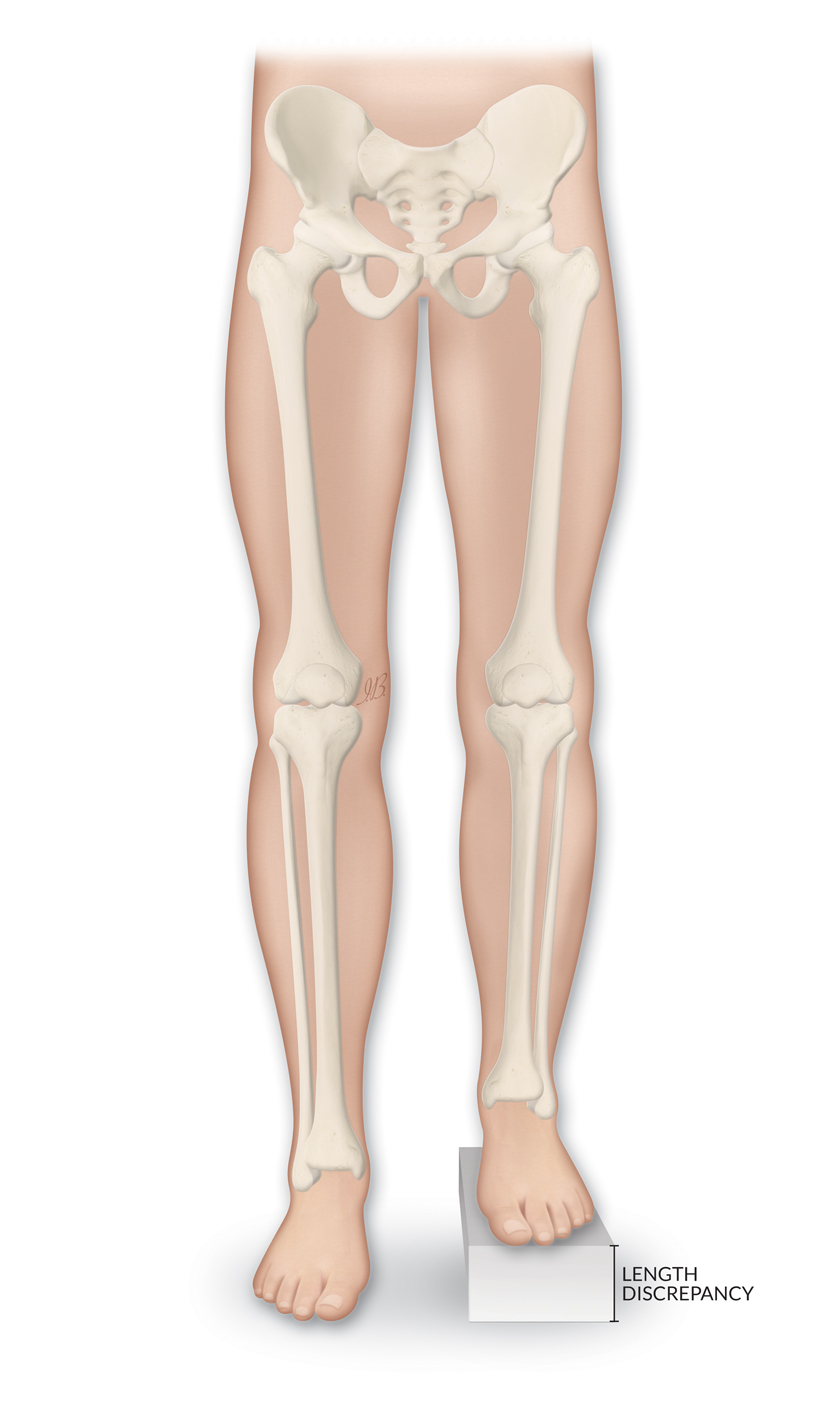
Leg Length Discrepancy (LLD) is a condition where one leg is shorter than the other. It is also known as anisomelia or limb length discrepancy. LLD is quite common in pediatric and adult individuals. It can be due to a condition that the person was born with (congenital), a condition developed during childhood and/or adolescence (developmental), or an acquired condition, such as infection, trauma, or cancer. When the discrepancy is less than 1-2 cm, it can be easily managed with an insole or a shoe raise, but a larger difference may require a different approach and more complex solutions.
Important safety information: Download the Product Instructions For Use.
The FitboneTM Intramedullary Limb-Lengthening System was developed in partnership with Professor Baumgart. The product was launched in 1997. Since then, this innovative treatment concept has grown into a global success story. The Fitbone TAA Intramedullary Lengthening system is intended for limb lengthening of the femur and tibia. With appropriate pre-operative planning, it is possible to ensure good limb alignment so that the limb is correct at the end of lengthening.
Important safety information: Download the Product Instructions For Use.
The Ilizarov System has experienced many modifications over the last fifty years. The TrueLok™ Ring Fixation System, developed at Texas Scottish Rite Hospital for Children (TSRHC) in Dallas, Texas, is one of the modern variants of the original fixator, but preserves many of the original principles of Professor Ilizarov. It consists of aluminum rings available in different sizes, connected to the bone through metal wires or/and bone screws. The relative movements of the rings allow the correction of almost all the bone deformities in upper and lower limbs and in the foot.
Important safety information: Download the Product Instructions For Use.
TL-HEX is a dynamic, 3D external fixation system that combines hardware and software to correct bone deformities. This hexapod-based system functions as a 3D bone segment-repositioning module. In essence, the system consists of circular and semi-circular external supports secured to the bones by wires and half-pins, interconnected by six struts.
Important safety information: Download the Product Instructions For Use.
The Orthofix Limb Reconstruction System™ (LRS) is a series of modular monolateral external fixators used in reconstructive procedures for treatment of short stature, bone loss, open fractures, non-union, and angular deformities.

LLD can be caused by congenital, developmental, or acquired conditions.
There are many congenital causes of LLD. This type of LLD is challenging to treat, not only due to the very young age of patients, but also because often there is a bigger discrepancy in leg length than with other causes, and this discrepancy increases as the child grows. It is important to have the help of a specialized surgical team, one that has experience with these cases.1, 2-7 Below you can find the most common congenital causes of LLD and a short description of each:
Developmental LLD is caused by conditions that are not present at birth, but that develop during childhood and/or adolescence. Bones grow only in a specific place, the physis (also known as the growth plate). Conditions or interventions that affect this growing part of the bone, such as infections, trauma or surgery, can cause LLD. The LLD may be subtle at first but will become more noticeable as the child/adolescent grows, especially because of the development of abnormal walking patterns.2-7
Below are some of the reasons for developmental LLD:
While the child is still growing, it is common for the difference in length of the two limbs to increase and become more noticeable over time. However, LLD is often asymptomatic, as the growing child adapts and may tiptoe on the short leg, or bend the long leg to compensate. Sometimes patients may complain of pain or fatigue in the back, hip or knee area due to the imbalance in muscle forces. There may be a bend in the spine (scoliosis) as the body tries to correct for the leg length difference. 5

Assessment of LLD requires a reliable clinical evaluation and accurate imaging including X-rays. Sometimes more specialized scans or opinions are required to diagnose the underlying cause and decide on the best treatment. 8
The choice of nonsurgical or surgical treatment depends on many factors, including the amount of discrepancy (the current and the expected difference once the child has fully grown) and if the patient is having problems.
A shoe raise should be worn to prevent secondary problems from the LLD, and may be the only treatment required if the LLD is not too prominent. However, it can be difficult to tolerate a big shoe raise, which would be required for larger discrepancies. If the expected difference is more than 2 cm, a surgical procedure to slow down the growth of the longer leg may be considered. This may involve a temporary surgical plate over the growing part of the bone, or permanent fusion of the growth plate.
If the final discrepancy is expected to be more than 5 cm, the option to lengthen the shorter leg may be discussed. This involves a big operation to break the shorter bone (osteotomy) and attach an external or implant an internal device to slowly grow the bone. 9 Children and adolescents can continue to go to school and socialize during this treatment; however, they will need multiple hospital appointments for physiotherapy.
The orthopedic surgeon will discuss these options with the family and consider the patient’s overall status. There can be some flexibility in the timing of the surgery to suit schooling and family life. 10

In time, untreated LLD may lead to painful arthritis of the leg joints and spine.
If children are treated at the right time, they may recover full and normal function. If they have surgery, the risks are greatest if they choose to have the shorter leg lengthened. Complications after surgery include an angular deformity of the leg, infections, fracture, problems with the bone failing to heal, or not healing in the intended position, joint subluxation and dislocation or failure of the bone to grow.
Since it is difficult to predict how much the child will continue to grow, there is no guarantee that having surgery will result in legs of equal length in adulthood. 11